If you or a loved one is living with diabetes, you likely already know that managing blood sugar is a full-time job. But there is another crucial part of the body that requires just as much attention, yet often goes overlooked until it’s too late: your feet.
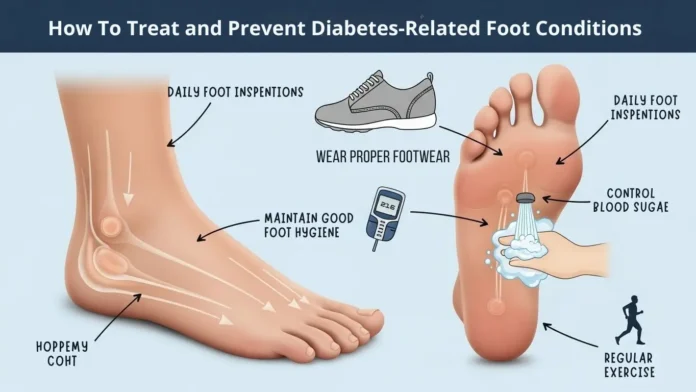
Foot complications are among the most serious and common issues for people with diabetes, but here is the good news: they are largely preventable. With the right daily routine diabetic foot care and a keen eye for warning signs, you can keep your feet healthy and active.
This guide covers everything you need to know about preventing potential issues and treating them effectively if they arise.
Why Does Diabetes Affect Your Feet
To protect your feet, it helps to understand exactly why they are vulnerable. High blood glucose levels over time can lead to two primary conditions that create a “perfect storm” for foot problems:
- Diabetic Neuropathy (Nerve Damage): High blood sugar can damage the nerves in your legs and feet. This often leads to a loss of sensation. You might step on a tack, develop a blister, or get a small cut and never feel it. Without pain as a warning system, minor injuries can worsen unnoticed.
- Peripheral Artery Disease (Poor Circulation): Diabetes often narrows the arteries, reducing blood flow to your extremities. Blood flow is essential for healing. If you have poor circulation, even a tiny cut can struggle to heal, increasing the risk of infection and ulcers.
The Ultimate Prevention Guide: Your Daily Routine
Prevention isn’t about drastic medical procedures; it’s about small, consistent habits. Think of this as your daily “maintenance check.”
The Daily Inspection
Because you might not feel an injury, you must see it. Check your feet every single day ideally in the evening when you take off your socks.
- Look for: Cuts, red spots, swelling, blisters, corns, or calluses.
- Check everywhere: Don’t forget the heels and between the toes.
- Use a tool: If you can’t lift your foot to see the bottom, place a mirror on the floor or ask a family member to help.
Wash and Dry with Care
- Warm, not hot: Nerve damage might make it hard to judge water temperature. Test the water with your elbow (not your foot!) before stepping in.
- Gentle washing: Use a soft washcloth and mild soap. Avoid scrubbing too hard.
- Dry thoroughly: This is critical. Fungal infections love moisture. Dry carefully between every toe.
Moisturize Smartly
Dry skin can crack, creating an entry point for bacteria. Apply a thin coat of lotion over the tops and bottoms of your feet.
- The Golden Rule: Never put lotion between your toes. The extra moisture there can lead to fungus or infection.
Nail Care
- Trim your toenails straight across. Curved corners can lead to ingrown toenails.
- File the edges gently with an emery board.
- Pro Tip: If you have poor eyesight or thick nails, see a podiatrist for nail trimming. It is not worth the risk of cutting yourself.
Footwear Your First Line of Defense
What you wear matters. Going barefoot is one of the biggest risks you can take inside your own home.
- The “Shake Out”: Before putting on your shoes, shake them out and feel inside for pebbles or rough seams. You might not feel a pebble with your foot, but it can cause a sore.
- Proper Fit: Buy shoes late in the day when your feet are naturally more swollen. Ensure there is plenty of room in the toe box so your toes aren’t squished.
- Socks Matter: Avoid socks with tight elastic bands at the top (which restrict blood flow) or thick, bulky seams that can rub against your toes. Look for seamless “diabetic socks” made of moisture-wicking material.
Recognizing the Red Flags
You should contact your doctor immediately if you notice any of the following. Do not wait to see if it “gets better on its own.”
- A blister, cut, or sore that hasn’t started to heal after a few days.
- Skin that feels warm to the touch (a sign of infection).
- Localized swelling or redness.
- A change in the shape of your foot.
- Pain, tingling, or a “pins and needles” sensation (often worse at night).
Treatment Options From Home Care to Medical Intervention
If you do develop a foot condition, swift treatment is vital to prevent serious complications like amputation.
Treating Minor Cuts at Home
If you find a minor scrape during your inspection:
- Clean it: Wash gently with mild soap and water.
- Cover it: Apply a sterile bandage. Avoid harsh antiseptics like hydrogen peroxide or iodine, which can damage the skin.
- Monitor it: Check it daily. If it isn’t healing or looks red, call your doctor.
Medical Treatments for Ulcers and Infections
If a wound becomes an ulcer (a deep open sore) or gets infected, your healthcare team may use several approaches:
- Off-loading: This involves taking pressure off the wound to let it heal. You may need to wear a special boot, cast, or surgical shoe, or use crutches/a wheelchair temporarily.
- Debridement: To help a wound heal, a doctor may need to remove dead or infected tissue. This reveals the healthy tissue underneath and stimulates healing.
- Antibiotics: If the wound is infected, oral or IV antibiotics are necessary.
- Revascularization: If poor circulation is preventing healing, a vascular surgeon may perform a procedure to clear blockages and restore blood flow to the leg.
Conclusion
Your feet carry you through life, and with diabetes, they need a little extra support. By combining daily inspections, proper footwear, and tight blood sugar control, you can drastically reduce the risk of foot complications. Remember, you are the most important member of your healthcare team—your daily vigilance is the best medicine.