Red Cell Distribution Width (RDW) is a crucial blood test marker that many people overlook until their doctor flags it as abnormal. If you’re reading this, chances are you’ve received blood work showing elevated RDW levels and you’re wondering whether you should be concerned. This comprehensive guide will help you understand exactly what RDW levels are dangerous, what they mean for your health, and what steps you should take.
What Is RDW and Why Does It Matter
RDW measures the variation in size of your red blood cells. Think of it this way: if you lined up all your red blood cells, RDW tells you how much they differ from each other in size. Healthy red blood cells should be relatively uniform in size, allowing them to efficiently carry oxygen throughout your body.
When RDW is elevated, it means your red blood cells vary significantly in size. Some are larger, some are smaller, and this variation disrupts their ability to transport oxygen effectively. Your body relies on consistent, healthy red blood cells to deliver oxygen to every tissue and organ, so significant size variation can signal underlying health problems.
Normal RDW Levels What You Should Expect
For most laboratories, normal RDW values fall between 11.5% and 14.5%. However, the exact reference range can vary slightly depending on the testing facility and the equipment used. Always compare your results to the specific reference range provided by your laboratory.
It’s important to understand that RDW is reported as a percentage. This percentage represents the coefficient of variation in red blood cell size. The higher the percentage, the greater the variation in cell size.
Some laboratories also report RDW-SD (standard deviation), which is measured in femtoliters (fL). Normal RDW-SD typically ranges from 39 to 46 fL. Both measurements assess the same concept but use different statistical methods.
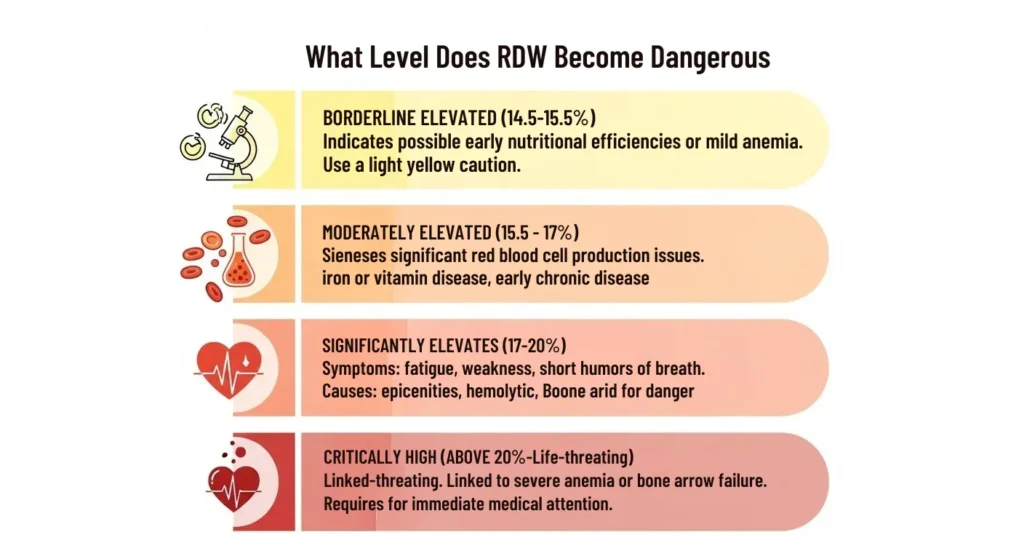
What Level Does RDW Become Dangerous
Understanding the danger zones of RDW requires looking at different elevation levels:
Why Elevated RDW Is Dangerous The Health Risks
The danger of high RDW extends beyond just abnormal blood cell sizes. Elevated RDW serves as a warning sign for multiple serious health tips conditions and has been linked to increased mortality risk.
Impaired Oxygen Delivery: When your red blood cells vary dramatically in size, they cannot efficiently bind and transport oxygen. Smaller cells have less hemoglobin capacity, while abnormally large cells may be fragile and break down prematurely. This leads to tissue hypoxia, where your organs and tissues don’t receive adequate oxygen to function properly.
Cardiovascular Complications: Multiple studies have established elevated RDW as an independent risk factor for heart disease complications. Research published in Circulation demonstrated that higher RDW values predict increased risk of cardiovascular events and death in patients with coronary disease. The relationship remains significant even after adjusting for other risk factors like age, cholesterol, and blood pressure.
Systemic Inflammation: Elevated RDW often reflects chronic inflammation throughout your body. Inflammatory processes interfere with iron metabolism, erythropoietin production, and red blood cell lifespan. This creates a cycle where inflammation causes RDW elevation, and the resulting inefficient oxygen delivery perpetuates inflammation.
Increased Mortality Risk: Perhaps most concerning, research in Archives of Internal Medicine found that elevated RDW independently predicts mortality across different age groups and disease states. Even in apparently healthy individuals, higher RDW values correlate with increased risk of death over time.
Medical Conditions That Cause Dangerous RDW Levels
Understanding what drives RDW elevation helps explain why certain levels are dangerous.
- Iron Deficiency Anemia: Most common cause, RDW >20% in severe cases
- Vitamin B12/Folate Deficiency: Causes megaloblastic anemia, large size variation
- Hemolytic Anemia: Premature RBC destruction, reticulocytosis
- Chronic Kidney Disease: Reduced erythropoietin, uremic toxins
- Cardiovascular Disease: Heart failure, CAD, inflammation, oxidative stress
- Cancer: Inflammation, marrow infiltration, chemo effects, anemia
- Liver Disease: Cirrhosis, hepatitis, disrupted RBC production
Symptoms That Accompany Dangerous RDW Levels
The symptoms you experience with elevated RDW depend on the underlying cause and severity. Higher RDW levels typically produce more noticeable symptoms:
Fatigue and Weakness: This is often the earliest and most common symptom. Reduced oxygen delivery to muscles and organs causes persistent tiredness that doesn’t improve with rest. You may find everyday activities exhausting.
Shortness of Breath: As RDW rises and oxygen delivery becomes less efficient, you may experience breathlessness with minimal exertion. In severe cases, you might feel short of breath even at rest.
Pale Skin and Mucous Membranes: Many conditions that elevate RDW also reduce hemoglobin levels. This causes pallor, particularly noticeable in the face, nail beds, and inner eyelids.
Rapid or Irregular Heartbeat: Your heart compensates for poor oxygen delivery by beating faster. You may notice palpitations, a racing heart, or an irregular rhythm.
Dizziness and Lightheadedness: Inadequate oxygen to the brain causes these symptoms, especially when standing up quickly or during physical activity.
Cold Hands and Feet: Poor circulation and reduced oxygen delivery to extremities cause persistent coldness in hands and feet.
Chest Pain: In severe cases, especially when RDW exceeds 18-20%, reduced oxygen delivery to heart muscle can cause chest discomfort or angina-like symptoms.
Cognitive Issues: Brain fog, difficulty concentrating, and memory problems can result from chronic oxygen deprivation to brain tissue.
When to Seek Immediate Medical Attention
While moderately elevated RDW warrants scheduled medical evaluation, certain situations require urgent care:
Seek emergency medical attention if you experience severe chest pain, extreme weakness that prevents normal activities, confusion or altered mental status, severe shortness of breath at rest, fainting or near-fainting episodes, or rapid heart rate with dizziness.
These symptoms combined with known elevated RDW may indicate severe anemia, heart complications, or other life-threatening conditions requiring immediate intervention.
Diagnostic Workup for Elevated RDW
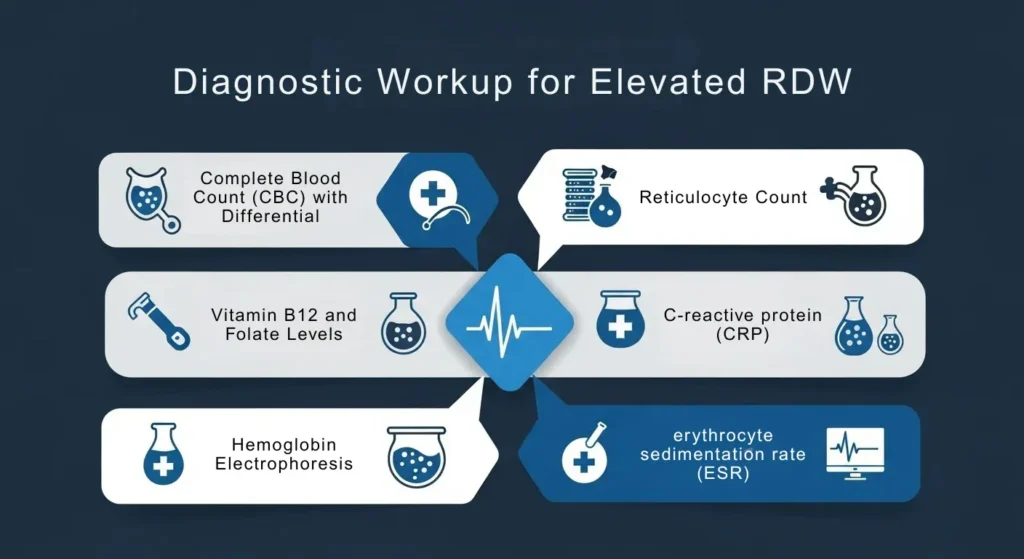
When your RDW is elevated, your healthcare provider will order additional tests to identify the cause:
| Test Name | Purpose / Description |
|---|---|
| Complete Blood Count (CBC) with Differential | Evaluates all blood cell types; includes hemoglobin, hematocrit, MCV, MCH, and WBC counts. |
| Iron Studies | Measures serum iron, ferritin, total iron-binding capacity (TIBC), and transferrin saturation to detect iron deficiency. |
| Vitamin B12 / Folate Levels | Identifies megaloblastic anemia; may include methylmalonic acid and homocysteine tests for borderline B12 levels. |
| Reticulocyte Count | Measures young red blood cells; high levels suggest blood loss or hemolysis, low levels suggest bone marrow dysfunction. |
| Peripheral Blood Smear | Microscopic examination of RBC shape and size; detects abnormalities such as sickle cell disease or thalassemia. |
| Kidney / Liver Function Tests | Assesses organ function that may influence RDW levels. |
| Inflammatory Markers (CRP, ESR) | Measures inflammation, which can correlate with elevated RDW. |
| Hemoglobin Electrophoresis | Identifies abnormal hemoglobin variants, including sickle cell disease and thalassemia. |
The Relationship Between RDW and Other Blood Markers
Understanding RDW requires examining it alongside other complete blood count parameters:
High RDW + Low MCV: This combination strongly suggests iron deficiency anemia. The low MCV indicates small red blood cells (microcytosis), while high RDW shows significant size variation as iron deficiency progresses.
High RDW + High MCV: This pattern indicates vitamin B12 or folate deficiency causing megaloblastic anemia. The cells are abnormally large and varied in size.
High RDW + Normal MCV: This can indicate a mixed deficiency (both iron and B12/folate), early-stage deficiency, or hemolytic anemia where destruction and production create varied cell sizes despite normal average size.
Normal RDW + Abnormal MCV: This pattern suggests thalassemia trait or chronic disease anemia, where cells may be uniformly small but without the variation seen in progressive deficiencies.
Treatment Approaches Based on RDW Levels
Treatment focuses on addressing the underlying cause of RDW elevation:
For Iron Deficiency (Most Common Cause):
- Oral iron supplementation: Typical doses range from 100-200mg of elemental iron daily. Ferrous sulfate, ferrous gluconate, or ferrous fumarate are common preparations.
- Take iron with vitamin C to enhance absorption and avoid taking with calcium, antacids, or tea which inhibit absorption.
- Dietary modifications: Increase intake of iron-rich foods including red meat, poultry, fish, beans, lentils, and fortified cereals.
- In severe cases or if oral iron isn’t tolerated or absorbed, intravenous iron may be necessary.
- Investigate and treat the source of iron loss, such as gastrointestinal bleeding or heavy menstrual periods.
For Vitamin B12 Deficiency:
- Oral B12 supplementation (1000-2000 mcg daily) works for most people.
- Intramuscular B12 injections may be needed initially for severe deficiency or absorption problems.
- Dietary sources include meat, fish, eggs, and dairy. Vegans should use fortified foods or supplements.
- Treat underlying absorption issues like pernicious anemia or intestinal disorders.
For Folate Deficiency:
- Folic acid supplementation (400-1000 mcg daily).
- Increase dietary folate through leafy greens, citrus fruits, beans, and fortified grains.
- Address alcohol consumption if excessive, as it interferes with folate metabolism.
For Chronic Disease:
- Optimize management of the underlying condition (kidney disease, heart failure, inflammatory disorders).
- Erythropoiesis-stimulating agents (ESAs) may be prescribed for anemia related to kidney disease or chemotherapy.
- Treat inflammation with appropriate medications when indicated.
For Hemolytic Anemia:
- Treatment varies based on cause: immunosuppressive therapy for autoimmune hemolysis, avoiding triggers in drug-induced cases, or supportive care for genetic conditions.
- Blood transfusions may be necessary for severe cases.
- Folic acid supplementation supports increased red blood cell production.
Monitoring and Follow Up
After treatment begins, regular monitoring ensures RDW levels return to normal:
Initial Follow-Up: Typically scheduled 4-6 weeks after starting treatment. This allows time for new red blood cells to be produced and RDW to show improvement.
Expected Improvement Timeline:
- Iron deficiency: RDW may initially worsen slightly as new small cells are produced, then improves over 8-12 weeks.
- B12/folate deficiency: Improvement often begins within 1-2 weeks with normalization in 2-3 months.
- Chronic disease: Improvement depends on controlling the underlying condition and may take several months.
Long-Term Monitoring: Once RDW normalizes, periodic rechecks ensure levels remain stable. Frequency depends on the underlying cause and risk of recurrence.
Prevention Strategies for Maintaining Healthy RDW
Preventing RDW elevation involves addressing common causes before they develop:
Nutritional Optimization:
- Maintain adequate iron intake: Men and postmenopausal women need 8mg daily; menstruating women need 18mg daily.
- Ensure sufficient B12: Adults need 2.4 mcg daily, with higher needs during pregnancy and for older adults.
- Get adequate folate: Adults need 400 mcg daily, with 600 mcg during pregnancy.
- Combine plant-based iron sources with vitamin C-rich foods to enhance absorption.
Address Bleeding Issues:
- Treat heavy menstrual bleeding through hormonal therapy or other interventions.
- Manage gastrointestinal issues like ulcers, hemorrhoids, or inflammatory bowel disease.
- Use caution with medications that increase bleeding risk, such as aspirin and NSAIDs.
Manage Chronic Conditions:
- Follow prescribed treatment plans for diabetes, kidney disease, heart disease, and inflammatory conditions.
- Regular monitoring allows early detection of complications affecting blood cell production.
Lifestyle Modifications:
- Limit alcohol consumption, which interferes with nutrient absorption and directly damages bone marrow.
- Avoid smoking, which increases oxidative stress and inflammation.
- Maintain a balanced diet rich in whole foods, fruits, vegetables, lean proteins, and whole grains.
Regular Health Screenings:
- Annual complete blood counts can detect RDW elevation before symptoms develop.
- This is particularly important if you have risk factors like chronic disease, dietary restrictions, or family history of blood disorders.
Special Populations and RDW Considerations
Certain groups require special attention regarding RDW levels:
Pregnant Women: Pregnancy increases iron and folate demands. RDW commonly rises during pregnancy due to increased blood volume and nutrient demands. However, values above 15% warrant investigation and supplementation.
Older Adults: Age-related changes in bone marrow function, medications, and chronic conditions make elevated RDW more common in elderly populations. Research shows RDW is a particularly strong mortality predictor in older adults.
Athletes: Intense training increases red blood cell turnover and iron loss through sweat and gastrointestinal stress. Athletes should monitor iron status and RDW, especially endurance athletes and females.
Vegetarians and Vegans: Plant-based diets provide less bioavailable iron and no vitamin B12 from natural sources. Regular monitoring and appropriate supplementation prevent deficiencies that elevate RDW.
Patients on Certain Medications: Medications like methotrexate, phenytoin, and some chemotherapy drugs interfere with folate metabolism and bone marrow function, potentially elevating RDW.
RDW as a Prognostic Marker
Beyond diagnosing anemia and nutritional deficiencies, RDW serves as a prognostic indicator across various conditions:
Research in Circulation established that elevated RDW independently predicts adverse outcomes in cardiovascular disease patients. Each 1% increase in RDW was associated with increased mortality risk, even after controlling for other cardiac risk factors.
Studies have shown that RDW predicts outcomes in heart failure, with higher values correlating with increased hospitalization rates and mortality. The marker helps risk-stratify patients for more intensive monitoring and treatment.
In critically ill patients, elevated RDW at hospital admission predicts increased mortality and longer hospital stays. This helps clinicians identify high-risk patients requiring more aggressive intervention.
Cancer patients with elevated RDW tend to have worse prognosis and lower survival rates across various cancer types. The marker reflects tumor burden, inflammation, and overall disease severity.
References:
- Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G. “Red blood cell distribution width: A simple parameter with multiple clinical applications.” Critical Reviews in Clinical Laboratory Sciences. 2015;52(2):86-105.
- Patel KV, Ferrucci L, Ershler WB, Longo DL, Guralnik JM. “Red blood cell distribution width and the risk of death in middle-aged and older adults.” Archives of Internal Medicine. 2009;169(5):515-523.
- Tonelli M, Sacks F, Arnold M, Moye L, Davis B, Pfeffer M. “Relation Between Red Blood Cell Distribution Width and Cardiovascular Event Rate in People With Coronary Disease.” Circulation. 2008;117(2):163-168.
- Lippi G, Targher G, Montagnana M, Salvagno GL, Zoppini G, Guidi GC. “Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients.” Archives of Pathology & Laboratory Medicine. 2009;133(4):628-632.
- Felker GM, Allen LA, Pocock SJ, et al. “Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank.” Journal of the American College of Cardiology. 2007;50(1):40-47.
- Koma Y, Onishi A, Matsuoka H, et al. “Increased red blood cell distribution width associates with cancer stage and prognosis in patients with lung cancer.” PLOS ONE. 2013;8(11):e80240.